We’re Stronger Together
With your help, we can make ambitious innovations in clinical care and education for our community.
Hematological malignancies (blood cancers) are caused by uncontrolled growth of abnormal blood cells, while non-cancerous blood disorders, genetic or metabolic disorders are caused by variations in DNA that affect healthy blood function.
If you’re fighting one of these conditions, your doctor may suggest Transplant and Cellular Therapy (TCT). Our TCT division offers treatments designed to replace, correct, and/or destroy unhealthy blood cells, supporting healthy cell regeneration. While these treatments are highly complex and require careful evaluation to see if they’re right for you, they have proven effective against a number of conditions.
Our Division of Transplant and Cellular Therapy/Hematological Malignancies is the only treatment program in our region to offer specialized TCT therapies for treating hematological malignancies (blood cancers), non-cancerous blood disorders, and other rare genetic and immune conditions.
We’re dedicated to treating the whole person — that means your physical, mental, and spiritual needs. Our team is here to support you every step of the way.
Hematological Malignancies (Blood Cancers)
Solid Tumors Requiring Treatment with Stem Cell Transplant or CAR-T cell therapy
Non-Cancerous Blood Disorders
Genetic or Metabolic Disorders
A bone marrow transplant (BMT), also known as a stem cell transplant, is a procedure that involves replacing diseased or damaged bone marrow — the soft tissue inside bones where blood cells are produced — with healthy stem cells that can help regenerate your bone marrow and restore normal blood cell production. This procedure is effective at treating leukemias, lymphomas, and multiple myeloma, as well as various non-cancerous blood disorders and genetic or metabolic disorders.
The first step of a bone marrow transplant is to collect healthy stem cells to replace the damaged ones. Healthy stem cells can either come from your own body (autologous transplant) or from a healthy donor match (allogeneic transplant) such as a sibling or unrelated individual. Next, you will undergo chemotherapy/radiation treatment to kill cancer cells and prepare your body for healthy cells. The collected stem cells are then infused into your body after chemotherapy or radiation to help regenerate healthy cells.
You should anticipate a hospitalization lasting 6-8 weeks to receive all the medicines to prepare your body for the stem cell transfusion and to allow your immune system to recover enough to safely leave the hospital after stem cell infusion. The stem cell infusion itself takes several hours. After the stem cell infusion, healthy cells will start to regenerate (engraftment), which can take weeks. You will need to stay in the hospital or visit an outpatient clinic daily during this critical phase of your treatment.
You might be a candidate for a bone marrow transplant if:
Bone marrow transplants can be lifesaving, but it’s important to know the risks. The process involves several stages, including preparation with intensive treatments (chemotherapy or radiation), the transplant itself, and a recovery phase where your immune system is rebuilt. Success depends on multiple factors such as your overall health, the quality of the donor match, and careful management of potential complications.
Chimeric antigen receptor CAR-T cell therapy harnesses the power of your own immune system to target and destroy cancer cells. It’s used to treat certain types of blood cancers, including acute lymphoblastic leukemia (ALL), non-Hodgkin lymphoma (NHL), and chronic lymphoblastic leukemia (CLL). CAR T-cell therapy is not yet widely available for all cancer types but is being studied for use in multiple myeloma and other cancers.
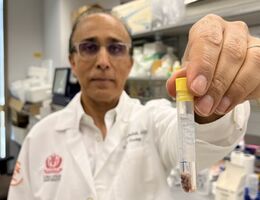
CAR T-cell therapy involves modifying your T-cells, a type of white blood cell that plays a crucial role in your immune system’s ability to fight infections and cancer. The T-cells are first collected from your bloodstream, genetically modified in the lab to help fight cancer cells, multiplied to create millions of these cells, and then reinfused back into your bloodstream via an IV to kill cancer cells directly.
Here’s a simplified, step-by-step breakdown of the process:
Receiving CAR-T cell therapy involves several stages, including evaluation and preparing you for treatment. You can expect a hospital stay of 6-8 weeks, during which time you will receive the infusion and be monitored for side effects. The total length of your hospital stay will depend on your specific situation.
You might be a candidate for CAR-T cell therapy if:
Gene therapy is an innovative FDA-approved treatment that works by correcting the body’s ability to make healthy red blood cells. The therapy is a curative treatment for diseases that cause unhealthy red blood cells, such as sickle cell disease or transfusion-dependent thalassemia. The stem cells are modified to either include genes for making healthy red blood cells or to increase the body’s ability to make a type of healthy red blood cell called fetal hemoglobin.
Gene therapy has several potential benefits, including reducing the need for blood transfusions and improving your overall quality of life. Gene therapy may also provide a long-term cure which allows your stem cells to make healthy red cells for life.
Your care team will collect a sample of your blood to identify and edit/replace the gene responsible for the disorder. Once the genetic change is made, the modified cells are returned to your body via infusion or injection into your bloodstream to start creating healthy blood cells.
Here’s a simplified, step-by-step breakdown of the process:
Receiving gene therapy involves several stages, such as evaluation and preparing you for treatment. You can expect a hospital stay of 4-6 weeks, during which time you will receive the infusion and be monitored for side effects. The total length of your hospital stay will depend on your specific situation.
If you’re fighting an inherited blood disorder such as sickle cell disease or thalassemia, gene therapy may be the ideal treatment for you. However, while early results of using gene therapy for blood disorders are promising, it’s still an evolving treatment. Your doctor will consider factors such as your age, overall health, and the severity of your condition when determining if this treatment is right for you.
We're here to support and guide you every step of the way. Your primary care physician or the emergency department may refer you to the Loma Linda University Cancer Center. If you'd like to receive treatment at our cancer center, ask your doctor for a referral.
Referring providers can contact us at 909-558-9602 or [email protected]



A bone marrow transplant (BMT), also known as a stem cell transplant, is a procedure that involves replacing diseased or damaged bone marrow — the soft tissue inside bones where blood cells are produced — with healthy stem cells that can help regenerate your bone marrow and restore normal blood cell production. This procedure is effective at treating leukemias, lymphomas, and multiple myeloma, as well as various non-cancerous blood disorders and genetic or metabolic disorders.
The first step of a bone marrow transplant is to collect healthy stem cells to replace the damaged ones. Healthy stem cells can either come from your own body (autologous transplant) or from a healthy donor match (allogeneic transplant) such as a sibling or unrelated individual. Next, you will undergo chemotherapy/radiation treatment to kill cancer cells and prepare your body for healthy cells. The collected stem cells are then infused into your body after chemotherapy or radiation to help regenerate healthy cells.
You should anticipate a hospitalization lasting 6-8 weeks to receive all the medicines to prepare your body for the stem cell transfusion and to allow your immune system to recover enough to safely leave the hospital after stem cell infusion. The stem cell infusion itself takes several hours. After the stem cell infusion, healthy cells will start to regenerate (engraftment), which can take weeks. You will need to stay in the hospital or visit an outpatient clinic daily during this critical phase of your treatment.
You might be a candidate for a bone marrow transplant if:
Bone marrow transplants can be lifesaving, but it’s important to know the risks. The process involves several stages, including preparation with intensive treatments (chemotherapy or radiation), the transplant itself, and a recovery phase where your immune system is rebuilt. Success depends on multiple factors such as your overall health, the quality of the donor match, and careful management of potential complications.
Chimeric antigen receptor CAR-T cell therapy harnesses the power of your own immune system to target and destroy cancer cells. It’s used to treat certain types of blood cancers, including acute lymphoblastic leukemia (ALL), non-Hodgkin lymphoma (NHL), and chronic lymphoblastic leukemia (CLL). CAR T-cell therapy is not yet widely available for all cancer types but is being studied for use in multiple myeloma and other cancers.
CAR T-cell therapy involves modifying your T-cells, a type of white blood cell that plays a crucial role in your immune system’s ability to fight infections and cancer. The T-cells are first collected from your bloodstream, genetically modified in the lab to help fight cancer cells, multiplied to create millions of these cells, and then reinfused back into your bloodstream via an IV to kill cancer cells directly.
Here’s a simplified, step-by-step breakdown of the process:
Receiving CAR-T cell therapy involves several stages, including evaluation and preparing you for treatment. You can expect a hospital stay of 6-8 weeks, during which time you will receive the infusion and be monitored for side effects. The total length of your hospital stay will depend on your specific situation.
You might be a candidate for CAR-T cell therapy if:
Gene therapy is an innovative FDA-approved treatment that works by correcting the body’s ability to make healthy red blood cells. The therapy is a curative treatment for diseases that cause unhealthy red blood cells, such as sickle cell disease or transfusion-dependent thalassemia. The stem cells are modified to either include genes for making healthy red blood cells or to increase the body’s ability to make a type of healthy red blood cell called fetal hemoglobin.
Gene therapy has several potential benefits, including reducing the need for blood transfusions and improving your overall quality of life. Gene therapy may also provide a long-term cure which allows your stem cells to make healthy red cells for life.
Your care team will collect a sample of your blood to identify and edit/replace the gene responsible for the disorder. Once the genetic change is made, the modified cells are returned to your body via infusion or injection into your bloodstream to start creating healthy blood cells.
Here’s a simplified, step-by-step breakdown of the process:
Receiving gene therapy involves several stages, such as evaluation and preparing you for treatment. You can expect a hospital stay of 4-6 weeks, during which time you will receive the infusion and be monitored for side effects. The total length of your hospital stay will depend on your specific situation.
If you’re fighting an inherited blood disorder such as sickle cell disease or thalassemia, gene therapy may be the ideal treatment for you. However, while early results of using gene therapy for blood disorders are promising, it’s still an evolving treatment. Your doctor will consider factors such as your age, overall health, and the severity of your condition when determining if this treatment is right for you.
We're here to support and guide you every step of the way. Your primary care physician or the emergency department may refer you to the Loma Linda University Cancer Center. If you'd like to receive treatment at our cancer center, ask your doctor for a referral.
Referring providers can contact us at 909-558-9602 or [email protected]



With your help, we can make ambitious innovations in clinical care and education for our community.