We’re Stronger Together
With your help, we can make ambitious innovations in clinical care and education for our community.
The cornea is the transparent part of the eye covering the iris, the pupil and anterior chamber. The cornea refracts light and helps with the focusing of the eye. Sometimes disease, scarring or other factors can impact the functionality of the cornea, reducing the amount of light entering your eye. A corneal transplant can help repair the cornea and correct the vision.
Keratoconus treatment depends on your symptoms. When your symptoms are mild, your vision can be corrected with eyeglasses. Later you may need to wear special hard contact lenses to help keep vision in proper focus.
To determine if corneal cross-linking may be right for you or a member of your family, please contact Jesica McCowen Refractive Coordinator (909) 558-2000.
Corneal transplantation is recommended for persons who have:
Sometimes, the body rejects the transplanted tissue. This occurs in a small number of patients.
Other risks for a corneal transplant include:
The risks for any anesthesia are:
The risks for any surgery are:
Full visual recovery may take up to 1 year. Most patients with successful corneal transplants will enjoy good vision for many years.
Call your doctor if you have any of the following symptoms. They may be signs of a complication.
Your doctor will give you an eye patch to wear for a short period of time. This protects the new cornea from injury. Carefully follow your doctor's instructions regarding eye drops after surgery, which may prevent rejection.
Countless people struggle for years from the discomfort and pain of dry eye disease. Dry eye is a common condition that occurs when your tears are not able to produce enough lubrication for your eyes. Tears can be inadequate and irregular for many reasons. While different products are available to manage dry eye disease, they only provide temporary relief.
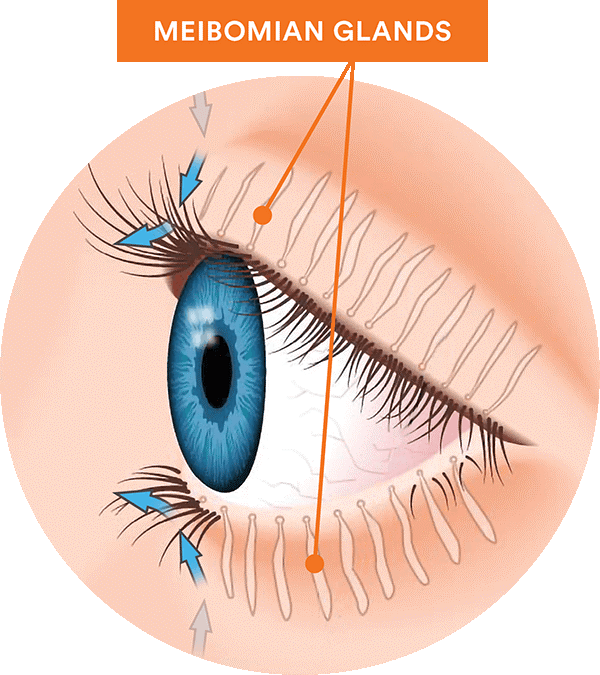
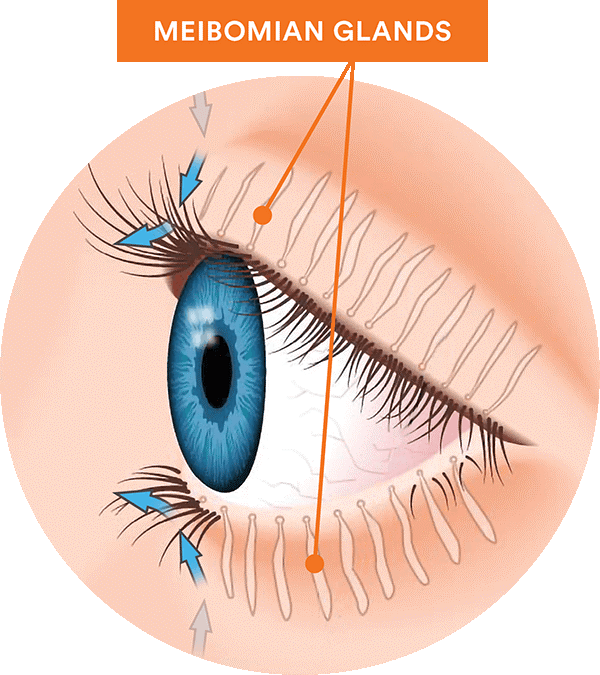
Meibomian gland dysfunction (MGD) is the leading cause of dry eye disease. MGD is a condition where your meibomian glands are not working correctly. These tiny oil glands are located in the upper and lower eyelids and secrete oil every time you blink. The oil is a major component of healthy tears, preventing tear film from evaporating.
MGD can cause dry eye symptoms, including throbbing, stinging and itching. You may also have MGD without any of these symptoms (known as asymptomatic MGD). If neglected, MGD may get worse over time.
Yes, there are effective treatments to reduce MGD’s long-term impact. The best treatment for you will depend on what’s causing your dry eye. Treatments include lubricant eye drops, omega-3 supplements, warm compresses, punctal plugs and LipiFlow.
LipiFlow is an automated treatment that helps clear away gland blockage and revive gland function. Our expert team provides the LipiFlow procedure in a single office visit in just 12 minutes. While the results vary from patient to patient, you can experience relief from dry eye symptoms for up to twelve months.
This procedure is preferred to the corneal transplant procedure (PKP) in appropriate patients due to a much faster recovery, and greatly decreased risks of complications. In treating patients with corneal endothelial dysfunction, the standard of care has been corneal transplant surgery (PKP), a procedure which replaces the full thickness of the cornea. With the exception of tissue quality and suturing techniques, few improvements have been made within the last 50 years. PKP has several well known disadvantages such as unpredictable refractive outcomes, a prolonged recovery that often takes a year, a permanent susceptibility to trauma, to mention a few.
Partial thickness corneal transplant (DSAEK) has been perfected over the last decade. In 1998, Dutch ophthalmologist Dr. Gerrit Melles developed a way to strip just Descemet's membrane from the cornea, and implant a manually dissected donor disc. The initial technique represented a definite improvement over PKP, but was very surgeon dependent, tedious, and required extensive manual dissection of the donor's cornea. More recently Dr. Mark Gorovoy automated endothelial keratoplasty using a microkeratome, making the corneal dissection very reproducible, like creating a LASIK flap. Automating the dissection creates a smoother surface on the donor cornea than what can be reliably obtained with a manual dissection. This translates in to a better optical interface.
The procedure starts by peeling off Descemet's membrane through a 4.5 mm limbal incision, leaving a smooth corneal host interface. The posterior donor tissue is then prepared with the microkeratome that, with a deep cut, removes the majority of the stroma. The posterior lamellar donor button consists of endothelium, Descemet's membrane, and 100 to 200um of stromal tissue. The donor disc is folded and inserted in the anterior chamber. The donor disc is then pressed into place with an air bubble, and remains fixed in place by the suction action of the endothelium.
The procedure is performed through a small limbal incision like that used for cataract surgery, no extensive corneal suturing is required. There is no risk of exposed or infected corneal sutures. Compared to PKP, there is much greater wound strength which is very important in elderly patients at risk of falling.
Postoperative care for DSAEK is similar, but less tedious than that of PKP for both surgeon and patient. Although techniques may differ slightly from surgeon to surgeon, most have found the results of DSAEK to be significantly better than PKP. Some consider it to be the standard of care for any patient suffering with Fuchs' corneal dystrophy, or post-cataract corneal decompensation. With DSAEK the speed of visual recovery is significantly improved. Typically the patient's vision recovers in 2 -to-4 months with BSCVA of 20/40 or better with little change in their spectacle correction. The refractive outcomes are far more predictable, since there is no significant induced astigmatism. Potentially, there is less risk of rejection.
Keratoconus treatment depends on your symptoms. When your symptoms are mild, your vision can be corrected with eyeglasses. Later you may need to wear special hard contact lenses to help keep vision in proper focus.
To determine if corneal cross-linking may be right for you or a member of your family, please contact Jesica McCowen Refractive Coordinator (909) 558-2000.
Corneal transplantation is recommended for persons who have:
Sometimes, the body rejects the transplanted tissue. This occurs in a small number of patients.
Other risks for a corneal transplant include:
The risks for any anesthesia are:
The risks for any surgery are:
Full visual recovery may take up to 1 year. Most patients with successful corneal transplants will enjoy good vision for many years.
Call your doctor if you have any of the following symptoms. They may be signs of a complication.
Your doctor will give you an eye patch to wear for a short period of time. This protects the new cornea from injury. Carefully follow your doctor's instructions regarding eye drops after surgery, which may prevent rejection.
Countless people struggle for years from the discomfort and pain of dry eye disease. Dry eye is a common condition that occurs when your tears are not able to produce enough lubrication for your eyes. Tears can be inadequate and irregular for many reasons. While different products are available to manage dry eye disease, they only provide temporary relief.
Meibomian gland dysfunction (MGD) is the leading cause of dry eye disease. MGD is a condition where your meibomian glands are not working correctly. These tiny oil glands are located in the upper and lower eyelids and secrete oil every time you blink. The oil is a major component of healthy tears, preventing tear film from evaporating.
MGD can cause dry eye symptoms, including throbbing, stinging and itching. You may also have MGD without any of these symptoms (known as asymptomatic MGD). If neglected, MGD may get worse over time.
Yes, there are effective treatments to reduce MGD’s long-term impact. The best treatment for you will depend on what’s causing your dry eye. Treatments include lubricant eye drops, omega-3 supplements, warm compresses, punctal plugs and LipiFlow.
LipiFlow is an automated treatment that helps clear away gland blockage and revive gland function. Our expert team provides the LipiFlow procedure in a single office visit in just 12 minutes. While the results vary from patient to patient, you can experience relief from dry eye symptoms for up to twelve months.
This procedure is preferred to the corneal transplant procedure (PKP) in appropriate patients due to a much faster recovery, and greatly decreased risks of complications. In treating patients with corneal endothelial dysfunction, the standard of care has been corneal transplant surgery (PKP), a procedure which replaces the full thickness of the cornea. With the exception of tissue quality and suturing techniques, few improvements have been made within the last 50 years. PKP has several well known disadvantages such as unpredictable refractive outcomes, a prolonged recovery that often takes a year, a permanent susceptibility to trauma, to mention a few.
Partial thickness corneal transplant (DSAEK) has been perfected over the last decade. In 1998, Dutch ophthalmologist Dr. Gerrit Melles developed a way to strip just Descemet's membrane from the cornea, and implant a manually dissected donor disc. The initial technique represented a definite improvement over PKP, but was very surgeon dependent, tedious, and required extensive manual dissection of the donor's cornea. More recently Dr. Mark Gorovoy automated endothelial keratoplasty using a microkeratome, making the corneal dissection very reproducible, like creating a LASIK flap. Automating the dissection creates a smoother surface on the donor cornea than what can be reliably obtained with a manual dissection. This translates in to a better optical interface.
The procedure starts by peeling off Descemet's membrane through a 4.5 mm limbal incision, leaving a smooth corneal host interface. The posterior donor tissue is then prepared with the microkeratome that, with a deep cut, removes the majority of the stroma. The posterior lamellar donor button consists of endothelium, Descemet's membrane, and 100 to 200um of stromal tissue. The donor disc is folded and inserted in the anterior chamber. The donor disc is then pressed into place with an air bubble, and remains fixed in place by the suction action of the endothelium.
The procedure is performed through a small limbal incision like that used for cataract surgery, no extensive corneal suturing is required. There is no risk of exposed or infected corneal sutures. Compared to PKP, there is much greater wound strength which is very important in elderly patients at risk of falling.
Postoperative care for DSAEK is similar, but less tedious than that of PKP for both surgeon and patient. Although techniques may differ slightly from surgeon to surgeon, most have found the results of DSAEK to be significantly better than PKP. Some consider it to be the standard of care for any patient suffering with Fuchs' corneal dystrophy, or post-cataract corneal decompensation. With DSAEK the speed of visual recovery is significantly improved. Typically the patient's vision recovers in 2 -to-4 months with BSCVA of 20/40 or better with little change in their spectacle correction. The refractive outcomes are far more predictable, since there is no significant induced astigmatism. Potentially, there is less risk of rejection.
With your help, we can make ambitious innovations in clinical care and education for our community.