Related Conditions & Treatments
Refractory Epilepsy
What is refractory epilepsy?
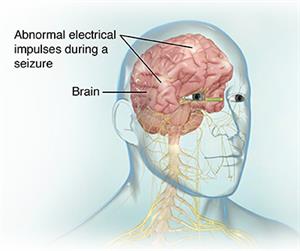
People with epilepsy have seizures. During a seizure, the nerve cells in the brain don't communicate like they should. The usual electrical activity in the brain changes. These seizures may last a few seconds or a few minutes.
Some people with epilepsy will have, or will one day develop, refractory epilepsy. This means that medicines don't work well, or at all, to control the seizures.
If you have refractory epilepsy, the type of seizures you have may affect your treatment. Seizures may be:
Generalized onset seizures. This means they involve both sides of your brain.
Focal onset seizures. This means seizure activity starts in a smaller part of your brain. It may later spread out to a wider area.
Unkown whether focal or generalized . This is when it has not yet been determined if seizures are focal or generalized for a person
Refractory epilepsy can have a big effect on your life. People with this type of epilepsy may have trouble at work or school. They may worry a lot about when their next seizure will come. They may also have injuries that result from their seizures. If your healthcare provider thinks you have refractory epilepsy, they may suggest that you visit a medical center that specializes in epilepsy.
What causes refractory epilepsy?
Some seizures have known causes, such as head injuries, infections, fevers, or brain tumors. But often the cause of seizures in epilepsy is not known.
In the same way, it is not clear why some people with epilepsy are not helped by antiseizure medicines. Or why these medicines sometimes stop working. The electrical activity in the brain during a seizure might get so high that medicines are no longer able to control it. But why this happens is not known.
What are the symptoms of refractory epilepsy?
The symptoms of a seizure can include:
Convulsions, or shaking movements
Loss of consciousness
Confusion
Tongue biting
Lip smacking
Loss of bowel or bladder control
Uncontrolled eye movements
Staring into space
Falling
Muscle rigidness, tremors, or twitching
Odd behavior (such as screaming or yelling)
If you still have seizures while you're taking medicine for them, you may have refractory epilepsy.
How is refractory epilepsy diagnosed?
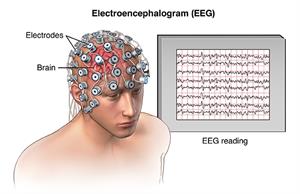
Your healthcare provider will likely ask you many questions about your seizures. You will likely also have a test called an electroencephalogram (EEG). This involves placing electrodes on your scalp to measure your brain's activity. Sometimes, the EEG can be watched for long spans of time at home or in the hospital.
Your healthcare provider may also want you to have a CT or MRI scan of your brain. Depending on the type of seizure activity and its location, you may need surgery. This would be done by a neurosurgeon who specializes in surgery for epilepsy. Your healthcare provider may do more tests like these to find out where your seizures are starting.
You will need to work closely with your healthcare provider to find out whether your epilepsy is refractory. Your provider may need to watch you closely during more seizures to try several medicines and combinations of medicines before they feel your condition is refractory. Your healthcare provider may want you to keep a daily journal of seizure activity and check in often to report your symptoms and any side effects as you try different medicine doses.
How is refractory epilepsy treated?
Your healthcare provider may suggest that you take other antiepilepsy medicine. You may take it alone or with other medicines you are already taking. There are many different medicines in this class. Some that may be tried are:
Carbamazepine
Phenytoin
Neurontin
Lamotrigine
Levetiracetam
Oxcarbazepine
Tiagabine
Topiramate
Zonisamide
Valproic acid
Vigabatrin
Clobazam
If medicines aren't helping with your seizures, you may need:
Surgery. Surgery may be very helpful if you have refractory partial epilepsy and the part of the brain where the seizures start can be found and safely removed. Your healthcare provider may advise surgery if you still have seizures after trying several antiepilepsy medicines. During the procedure, a surgeon who specializes in epilepsy surgery will take out the part of your brain that's starting the seizures.
Vagal nerve stimulation. If you can't have or don't want brain surgery, your healthcare provider may suggest vagus nerve stimulation with an implantable device. The device is placed under your skin in your chest. Wires connect it to the vagus nerve in your neck. It sends a current to the nerve. With this device, you may have fewer seizures. It may also help lessen the severity of a seizure that has already started.
Ketogenic diet. A special diet that may help some people control their seizures. This type of diet is high in fats and low in carbohydrates. If you follow this diet, you will need to work closely with your healthcare provider and take supplements of certain nutrients as needed.
Brain pacing. This is a newer treatment in which the brain is stimulated through wires (Deep brain stimulator or responsive neurostimulator) to prevent or stop seizures.
Can refractory epilepsy be prevented?
It might not be possible to prevent all of your seizures. But it is very important to use medicines exactly as your healthcare provider directs. Using your medicines the right way may help them work better to control your condition.
Living with refractory epilepsy
Living with refractory epilepsy can be hard. People with this health problem may worry a lot about when their next seizure will come. They may have trouble at work or school. They may no longer be allowed to drive. They may also have injuries that result from their seizures. It is important to do what you can to limit your chances of injury.
When should I call my healthcare provider?
Be sure to talk with your healthcare providers about when you should call. They will likely tell you to call if:
You continue to have seizures.
Your seizures become worse in intensity or frequency.
You have new symptoms during or after your seizures.
Call 911
Call 911 if you:
Have difficulty breathing or waking after the seizure
The seizure lasts longer than 5 minutes
You have back-to-back seizures
Key points about refractory epilepsy
Refractory epilepsy occurs when your antiepilepsy medicines are no longer controlling your seizures. Often the cause of refractory epilepsy is not known.
Your healthcare provider will likely give you other medicines to try to get your seizures under control. If this does not work, other choices may be surgery to remove the part of the brain where the seizures start or electrical stimulation of a nerve leading to the brain.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your provider tells you.
At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you do not take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your healthcare provider if you have questions, especially after office hours or on weekends.