Related Conditions & Treatments
Bladder Cancer: Introduction
What is cancer?
Cancer starts when cells in the body change (mutate) and grow out of control. To help you understand what happens when you have cancer, let's look at how your body works normally. Your body is made up of tiny building blocks called cells. Normal cells grow when your body needs them. They die when your body doesn't need them any longer.
Cancer is made up of abnormal cells that grow even though your body doesn't need them. In most cancers, the abnormal cells grow to form a lump or mass called a tumor. If cancer cells are in the body long enough, they can grow into (invade) nearby tissues. They can even spread to other parts of the body (called metastasis).
What is bladder cancer?
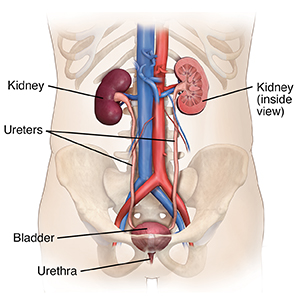
The bladder is a hollow, balloon-like organ in the lower belly (pelvis). It holds urine until it’s passed out of the body. Urine comes into the bladder through 2 tubes called the ureters. Each ureter is attached to a kidney. This is where urine is made. When you pass urine, it comes out through a tube called the urethra. All of these organs make up the urinary tract.
The cell where the cancer starts
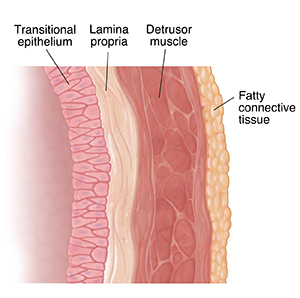
One way to discuss bladder cancer is to describe the kind of cells it starts in. The bladder wall is made up of many layers of cells. It has an outer layer of muscle cells and an inner lining layer of transitional cells. Bladder cancer can affect any one or all of these cells (and layers). These are the 3 types of cells that most commonly become bladder cancer:
-
Urothelial cells or transitional cells. These cells make up the tissue that lines the inside of the bladder. This tissue is called the urothelium. Cancer that starts here is called urothelial carcinoma or transitional cell carcinoma (TCC). This is, by far, the most common type of bladder cancer.
-
Squamous cells. These look like cells from the surface of the skin. They can start in the bladder if there's a lot of inflammation. Over time, they can become cancer. This type is rare, causing less than 1 in 50 of all bladder cancers.
-
Cells that make up glands. This type of bladder cancer is called adenocarcinoma. It’s very rare. Only about 1 in 100 people with bladder cancer has this type.
In rare cases, other cancers can start in the bladder. These include lymphoma, sarcoma, and small cell carcinoma.
How deep is the cancer in the bladder wall
Another way to talk about bladder cancer is by how deeply it spreads into the layers of the bladder wall. This puts the cancer into 1 of 2 groups:
- Nonmuscle invasive. This type of cancer affects only the inner lining of the bladder. (It's urothelial carcinoma or transitional cell carcinoma.) It hasn't grown deeper into the bladder's muscle layer. After treatment, nonmuscle invasive bladder cancer often comes back, often as another nonmuscle invasive cancer.
- Muscle invasive. This cancer affects deeper muscle layers of the bladder and maybe the fatty tissue around the bladder. Invasive bladder cancer is more likely to spread to nearby organs. These can include the kidneys, prostate gland, and the uterus and vagina. It may also spread to the lymph nodes. Lymph nodes are small groups of special cells that fight infections. Almost all squamous cell bladder cancers and adenocarcinomas are invasive.
Subtypes of transitional cell carcinomas
Transitional cell carcinomas (TCCs) may also be described as being either papillary or flat:
-
Papillary tumors. These look like small mushrooms and grow into the open part of the bladder. They rarely go deeper into other layers of the bladder. Some types of papillary tumors tend to come back. But they can be removed without damaging the bladder.
-
Flat tumors. These don't grow into the open part of the bladder. They spread along the lining.
If either of these grow into the deeper layers of the bladder, it's called invasive TCC.
Talk with your healthcare provider
If you have questions about bladder cancer, talk with your healthcare provider. Your provider can help you understand more about this cancer.