Abdominal Aortic Aneurysm
What is an abdominal aortic aneurysm?
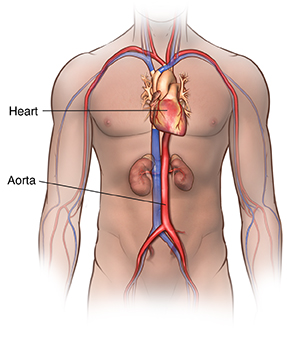
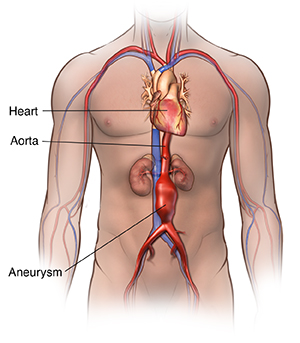
The aorta is the largest blood vessel in the body. It brings oxygenated blood from the heart to the rest of the body. An aortic aneurysm is a bulging, weakened area in the wall of the aorta. Over time, the blood vessel swells and is at risk for bursting (rupture) or separating (dissection). This can cause life-threatening bleeding and possibly death.
Aneurysms occur most often in the part of the aorta that runs through the belly (abdomen). This is called an abdominal aortic aneurysm (AAA). A thoracic aortic aneurysm refers to the part of the aorta that runs through the chest.
Once formed, an aneurysm will slowly get larger and weaker.
What causes an abdominal aortic aneurysm?
Many things can cause the breakdown of the aortic wall tissues and lead to an AAA. Experts don’t know the exact cause. But they believe atherosclerosis plays an important role. Atherosclerosis is a buildup of plaque. This is a deposit of fatty substances, cholesterol, cellular waste products, calcium, and fibrin in the inner lining of an artery. Risk factors for atherosclerosis include:
Being older than 60
Being male (men are more likely to develop an AAA than women)
Family history of the disease in a parent or sibling
Genetic factors
High cholesterol
High blood pressure
Smoking
Diabetes
Obesity
Other diseases that may cause an AAA include:
Connective tissue disorders, such as Marfan syndrome, Ehlers-Danlos syndrome, Turner's syndrome, and polycystic kidney disease
Defects that are present at birth (congenital), such as bicuspid aortic valve or coarctation of the aorta
Inflammation of the temporal arteries and other arteries in the head and neck
Injury
Infection, such as syphilis, salmonella, or staphylococcus (rare)
Men ages 65 to 75 who have ever smoked should have a one-time ultrasound screening for AAA. If you are a male age 65 to 75 and have never smoked, your healthcare provider may advise screening based on other risk factors, such as your health history or family history.
What are the symptoms of an abdominal aortic aneurysm?
In most cases, abdominal aortic aneurysms don't cause symptoms. An aneurysm may be found by an X-ray, CT scan, or MRI that was done for other reasons. Since an AAA may not have symptoms, it's called the silent killer. It may rupture before being diagnosed.
Pain is the most common symptom of an abdominal aortic aneurysm. The pain linked to an AAA may be found in the abdomen, chest, lower back, or groin area. The pain may be severe or dull. Sudden, severe pain in the back or abdomen may mean the aneurysm is about to burst. This is a life-threatening medical emergency.
An AAA may also cause a pulsing feeling, like a heartbeat, in the abdomen.
The symptoms of an AAA may look like other health conditions or problems. Always get medical care right away if you think you have an AAA.
How is an abdominal aortic aneurysm diagnosed?
Your healthcare provider will do a complete health history and physical exam. Other possible tests include:
CT scan. This test uses X-rays and computer technology to make horizontal, or axial, images (often called slices) of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than standard X-rays.
MRI. This test uses a combination of large magnets, radiofrequencies, and a computer to make detailed images of organs and structures within the body.
Echocardiogram. This test (also called echo) evaluates the heart’s structure and function. It uses sound waves recorded on an electronic sensor. This makes a moving picture of the heart and heart valves, as well as the structures in the chest. These include the lungs and the area around the lungs and the chest organs.
Transesophageal echocardiogram (TEE). This test uses echocardiography to check for an aneurysm and check the heart valves. It can also see if there is a tear in the aorta lining. TEE is done by inserting a probe with a transducer on the end down into the throat.
Chest X-ray. This test uses invisible electromagnetic energy beams to make images of internal tissues, bones, and organs onto film.
Arteriogram (angiogram). This is an X-ray image of the blood vessels. It's used to assess conditions, such as aneurysm, narrowing of the blood vessel, or blockages. A dye (contrast) is injected through a thin, flexible tube placed in an artery. The dye makes the blood vessels easy to see on an X-ray.
Ultrasound. An ultrasound uses high-frequency sound waves and a computer to create images of blood vessels, tissues, and organs. An ultrasound is used to view internal organs as they function. And it is used to evaluate blood flow through various vessels.
How is an abdominal aortic aneurysm treated?
Treatment will depend on how bad the aneurysm is and if there are symptoms. Treatment may include:
Monitoring with MRI or CT. These tests are done to check the aneurysm’s size and how fast it’s growing.
Managing risk factors. Making some lifestyle changes may help control the progression of the aneurysm. These include quitting smoking, controlling blood sugar if you have diabetes, losing weight if overweight, controlling blood pressure, and eating a healthy diet.
Medicine. This can control factors such as high cholesterol or high blood pressure.
Surgery
Abdominal aortic aneurysm open repair. A large cut (incision) is made in the belly to let the surgeon see and fix the AAA. A mesh, metal coil-like tube called a stent or graft may be used. This graft is sewn to the aorta. It connects one end of the aorta at the site of the aneurysm to the other end.
Endovascular aneurysm repair (EVAR). EVAR needs only small cuts in the groin. Using X-ray guidance and specially-designed tools, the surgeon can fix the aneurysm by inserting the stent or graft inside the aorta. The graft material may cover the stent. The stent helps hold the graft open and in place.
A small aneurysm or one that doesn't cause symptoms may not need surgery until it reaches a certain size. Or until it's quickly growing over a short time period. Your healthcare provider may recommend watchful waiting. This may include having an ultrasound, duplex scan, or CT scan every 6 months to closely watch the aneurysm. Blood pressure medicine may be used to control high blood pressure.
If the aneurysm is causing symptoms or is large, your provider may recommend surgery.
What are possible complications of an abdominal aortic aneurysm?
A serious complication of an AAA is an aortic dissection. This is a tear in the aortic lining. It can occur anywhere along the aorta. Aortic dissection can be a life-threatening emergency. The most common symptom of an aortic dissection is sudden severe, constant chest or upper back pain. This is sometimes described as ripping or tearing. The pain may move from one place to another.
When a diagnosis of aortic dissection is confirmed, immediate surgery or stenting is often done. Talk with your provider about how you can manage your AAA and reduce your risk for complications.
Another serious complication is rupture. When this occurs, it's a surgical emergency.
In most cases, AAAs don't cause symptoms. An aneurysm may be found by an imaging test that was done for other reasons.
Key points about abdominal aortic aneurysm
The aorta is the largest blood vessel in the body. An aortic aneurysm is a bulging, weakened area in the wall of the aorta.
An abdominal aortic aneurysm (AAA) is an aneurysm that occurs in the part of the aorta that runs through the abdomen.
Experts don’t know the exact cause. But they believe plaque buildup in the artery (atherosclerosis) plays an important role.
Since an AAA may not have symptoms, it's called the silent killer. The blood vessel may burst before being diagnosed. This can cause life-threatening bleeding and possibly death.
A serious complication is an aortic dissection. This is a tear in the aortic lining that can occur anywhere along the aorta. This can be a life-threatening emergency.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
Know the reason for your visit and what you want to happen.
Before your visit, write down questions you want answered.
Bring someone with you to help you ask questions and remember what your provider tells you.
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
Ask if your condition can be treated in other ways.
Know why a test or procedure is recommended and what the results could mean.
Know what to expect if you do not take the medicine or have the test or procedure.
If you have a follow-up appointment, write down the date, time, and purpose for that visit.
Know how you can contact your healthcare provider if you have questions, especially after office hours or on weekends and holidays.